¿Uña micótica o psoriasis ungueal?
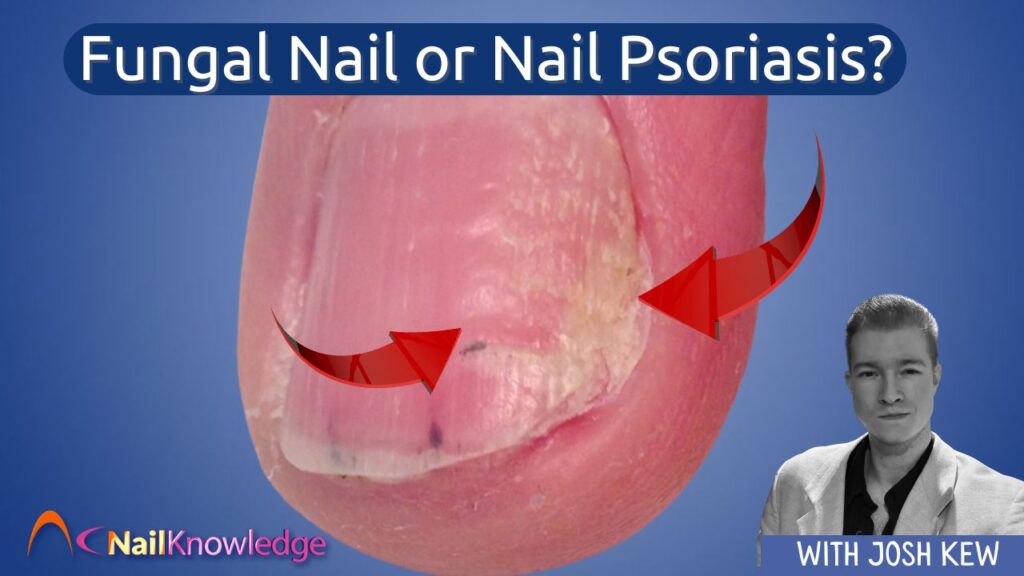
How Nail Pros Can Spot the Difference between Fungal Nail and Nail Psoriasis… and when to Refer
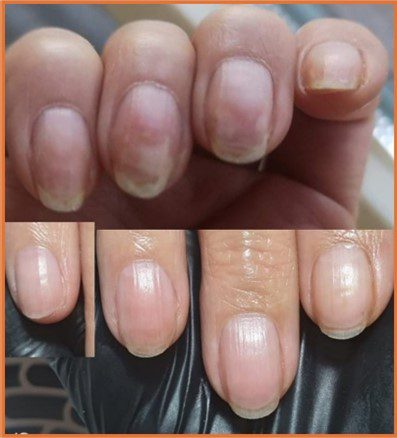
As a nail professional, your clients trust you to notice changes in their nails, and you’re often the first to spot signs of something unusual. Two of the most commonly confused conditions are fungal nail infections and nail psoriasis. Both can cause discolouration, thickening, and uña escamosa superficies, pero requieren enfoques muy diferentes.
Knowing what to look for and when to refer to a podiatrist can make a big difference to your clients’ nail health.
¿Qué es una infección por hongos en las uñas?
Una infección por hongos en las uñas (también conocida como onicomicosis) is caused by a buildup of dermatophyte mould fungi that invade the nail plate, the skin underneath it (the nail bed) or any or all of the skin of the foot itself. These organisms thrive in warm, moist environments and often begin by infecting the skin between the toes (athlete’s foot) before spreading to the toenails.

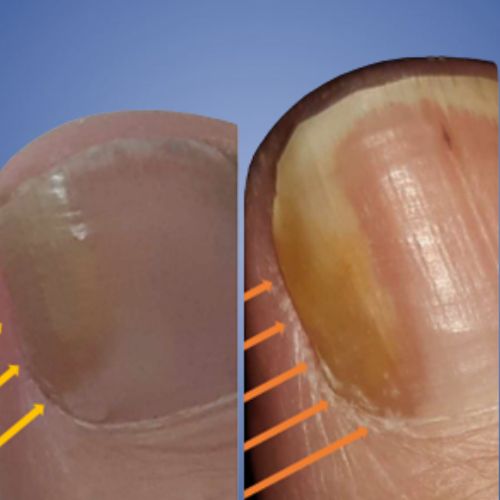

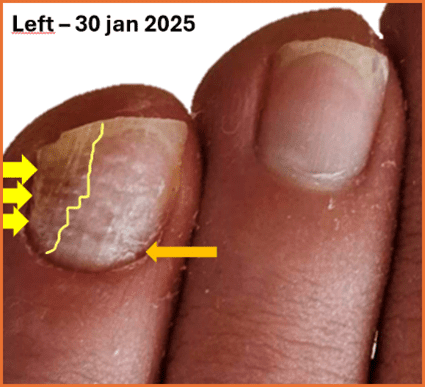

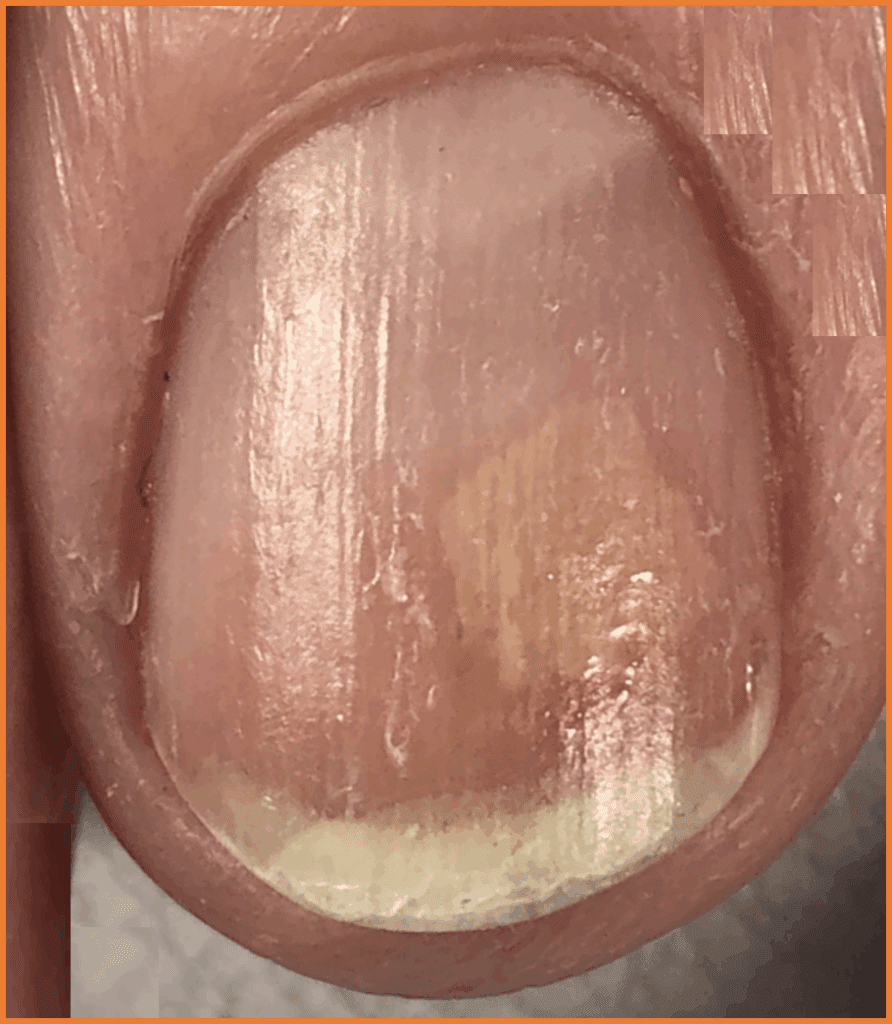
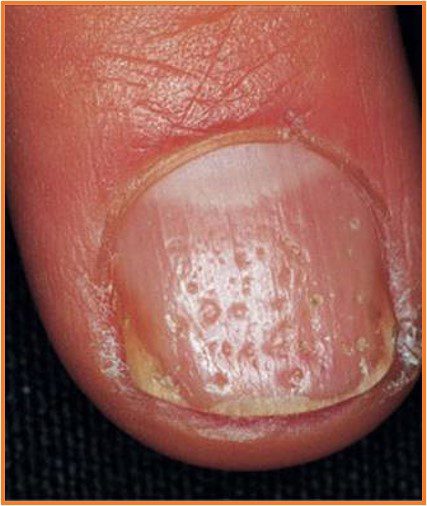
Fig D1 y Fig D2: Looks like Psoriasis – It was tested and it’s a fungal infection but in this case, it could also be Psoriatic!
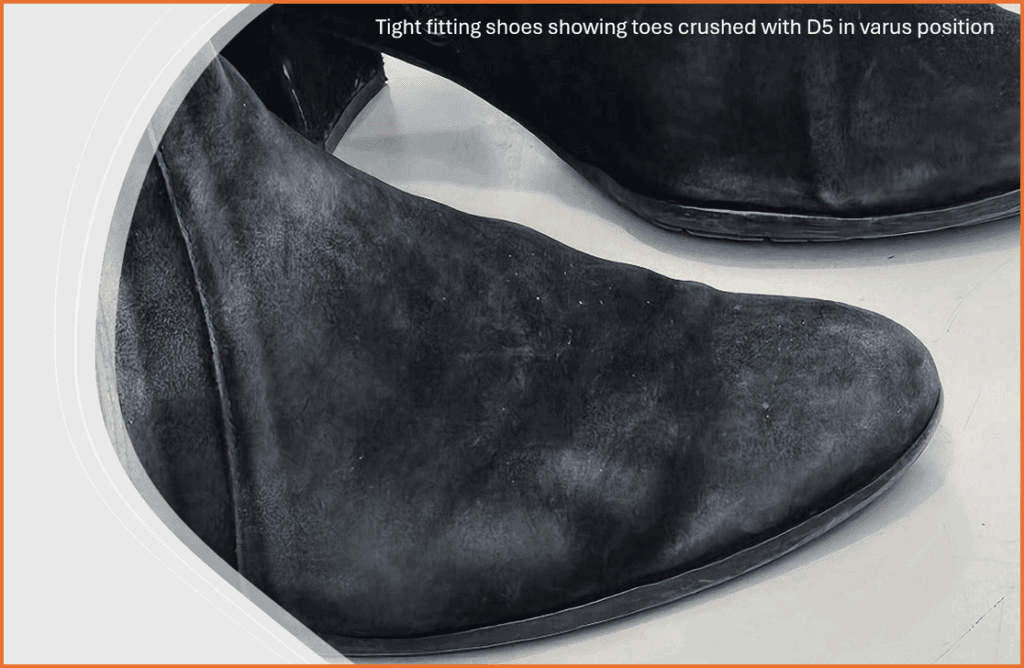
Fungal infections are contagious and can spread through shared footwear, nail tools, or damp environments like swimming pools, gyms and even your shower at home. Although a fungal infection can affect one or multiple nails, it may slowly worsen over time without treatment. You don’t have to be old to get one as fungal infections are often seen in young footballers or runners, the reason for this is damage to the unidad de clavos al correr o jugar, generalmente mini traumatismos de algún tipo que dan a los hongos la oportunidad de arraigar, pero incluso un calzado demasiado pequeño puede causar una abertura en una placa ungueal que los hongos pueden hacer su hogar.
¿Qué es la psoriasis ungueal?
La psoriasis es una enfermedad inflamatoria de la piel de larga duración que también puede afectar a alguna o a todas las partes de las uñas.s. In nail psoriasis, the immune system speeds up the production of skin cells around and under the nail, leading to a build-up of cells and abnormal nail growth.
La psoriasis ungueal es no contagioso, but it can be distressing and may lead to discomfort or changes in nail appearance. It may affect just the nails or be part of wider symptoms of psoriasis on the skin or even in the joints (psoriatic arthritis).
Qué aspecto tienen las infecciones por hongos en las uñas
Las infecciones por hongos en las uñas suelen comenzar en la punta o en un lateral de la uña y se extienden lentamente.
Signos comunes:
- Decoloración amarilla, marrón o blanca
- Desmenuzable o uña quebradiza bordes
- Uñas engrosadas
- Nail lifting from the nail bed (onycholysis)
- Restos escamosos bajo la uña
- Olor a humedad o desagradable
A menudo relacionado con:
- Traumatismo ungueal
- Llevar calzado apretado, no transpirable o mal ajustado.
- Athlete’s foot (tinea pedis)
- Andar descalzo por las zonas comunes
- Compartir herramientas para uñas
Aspecto de la psoriasis ungueal
La psoriasis ungueal puede afectar a todas las partes de la uña o a algunas de ellas. matriz de uñas (which forms the nail plate) or the nail bed (beneath the nail). It can appear even if the client doesn’t have visible psoriasis on the skin.
Signos comunes:
- Pequeñas picaduras (abolladuras diminutas) en la lámina ungueal
- A salmon-pink “oil drop” patch under the nail
- Crestas o surcos a lo largo de la uña
- Thickened skin under the nail (subungual hyperkeratosis)
- Manchas blancas o hemorragias en astilla
- Nails lifting from the nail bed, often across multiple nails
Las alteraciones psoriásicas de las uñas suelen ser simétricas y pueden afectar a una o varias uñas a la vez.
Por qué es importante
Estas dos afecciones pueden tener un aspecto muy similar, pero las causas y los tratamientos son completamente distintos. It’s impossible to diagnose either with just the eye – Fungal infections can only be properly diagnosed with a test – Psoriasis needs to be diagnosed by a Dermatologist.
Treating a fungal nail with antifungal won’t help if the problem is actually psoriasis. Likewise, treating nail psoriasis with topical steroids or an antifungal product won’t touch a fungal infection.
That’s why it’s essential to refer clients to a podiatrist if you see any persistent changes or signs of infection.
***Las pruebas pueden excluir o confirmar una infección fúngica.
Cuándo remitir a su cliente
Remitir a un podólogo si su cliente tiene:
- Dolor, hinchazón, sangrado o sensibilidad alrededor de la uña
- Uñas que huelen mal o parecen infectadas
- Symptoms that aren’t improving after self-treatment
- Cambios en varias uñas, especialmente si parecen simétricas
- Antecedentes personales o familiares de psoriasis o afecciones cutáneas
- Any unusual or concerning changes you’re unsure about
A podiatrist can take a nail sample, test for fungal infection, and make a clear diagnosis. They’ll also create a treatment plan tailored to your client’s needs.
Cómo ayudar
You’re not expected to diagnose, but you son in the perfect position to notice early changes. Your trained eye, paired with good hygiene and proper referrals, plays a huge role in protecting your client’s well-being.
By referring to a podiatrist when something doesn’t seem right, you’re giving your clients the best care possible and helping them get the treatment they need sooner rather than later.
Reflexión final
Nail health is about more than just looks. Whether it’s fungus or psoriasis, catching it early can prevent long-term damage and give your client peace of mind. If something doesn’t look right, trust your instincts and refer to a podiatrist. You could be the first person to make a real difference in their health journey.
*** 1.Tsunemi Y, Takehara K, Miura Y, Nakagami G, Sanada H, Kawashima M. Screening for tinea unguium by Dermatophyte Test Strip. Br J Dermatol. 2014;170(2):328-31.