Cómo detectarlo, detenerlo, tratarlo y cuándo acudir al podólogo
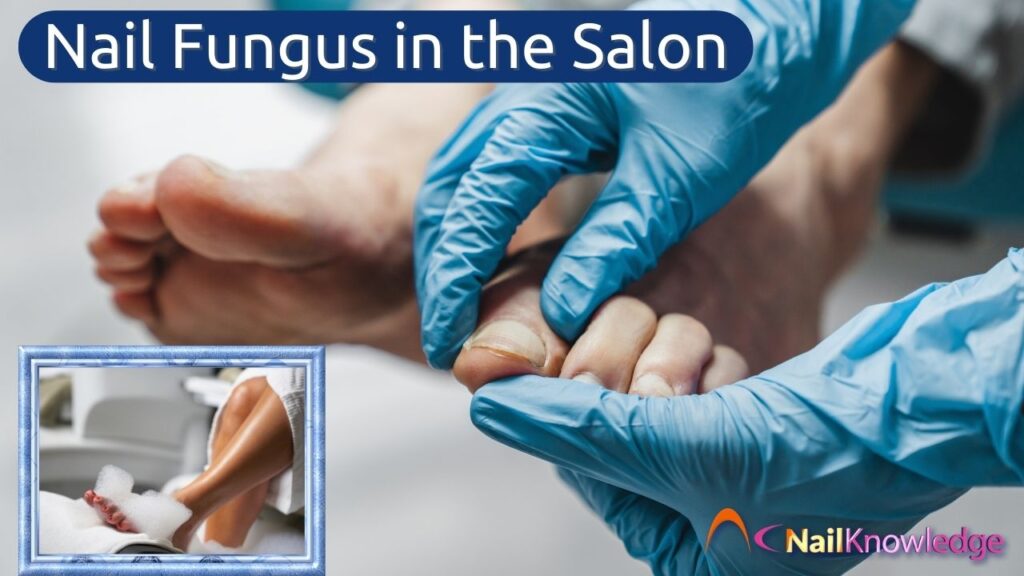
If you work in a nail salon, chances are you’ve encountered nail fungus in the salon without even realising it. These infections, known as onychomycosis, are more common than many people think. Although they aren’t immediately dangerous, they can be persistent and unsightly, making them difficult to eradicate. This underscores the importance of early detection and effective management, especially in a salon setting where hygiene is critical.
So, how do you spot nail fungus early, what should you do if a client has it, and when is it time to refer them to a podiatrist? Let’s break it all down, step by step.
Qué son los hongos de las uñas (onicomicosis)
Nail fungus (onychomycosis) is a slow-growing infection caused by fungal organisms called dermatophytes. These fungi feed on keratin, one of the proteins that makes up nails and skin, leading to thickened, discoloured, and often uñas quebradizas.
La infección puede comenzar en una uña y, si no se trata, puede extenderse a otras, incluidas las uñas de las manos, aunque las de los pies se ven afectadas con mucha más frecuencia.
But here’s the kicker: nail fungus is stubborn. It doesn’t clear up on its own and often requires months of treatment. That’s why early detection and proper management are so important especially in a salon setting where hygiene is everything.
Cómo identificar los hongos de las uñas en el salón de belleza
En las primeras fases, hongos en las uñas infections can be sneaky. They don’t always scream “Hey, I’m a fungal infection!” Por el contrario, suelen empezar de forma leve, con una ligera decoloración en algún lugar de la uña o alrededor de ella. lecho ungueal. Sin embargo, con el tiempo se hacen mucho más evidentes.
Signos y síntomas a tener en cuenta:
- Decoloración – Yellow, white, or brown patches on the nail. Some nails may even appear greenish or black in severe cases.
- Espesamiento – The nail may become unusually thick, making it difficult to cut.
- Fragilidad – The edges of the nail may crumble, split, or break away easily.
- Lifting (Onycholysis) – The nail may separate from the nail bed, creating a gap where dirt and bacteria can collect.
- Distorsión – The shape of the nail may change, becoming more curved or uneven.
- Olor – In some cases, fungal nails can develop a slightly unpleasant smell.
Fungal nails don’t always cause pain, but if the infection progresses, the thickened nail can press against shoes, leading to discomfort or even secondary bacterial infections.
Diagnóstico diferencial: ¿se trata realmente de una infección fúngica?
Not every thick, discoloured, or damaged nail is caused by fungus. As a nail technician, it’s important to know the difference between a fungal infection and other conditions that can mimic it.
Afecciones que pueden parecerse a los hongos de las uñas:
- Trauma – Repeated pressure from tight shoes or injury can cause thickening, white patches, and even nail detachment.
- Psoriasis – Psoriatic nails often have pitting (small dents), thickening, and a yellowish or red discolouration.
- Eczema & Other Skin Conditions – These can cause brittle, flaky nails that may look similar to fungal infections.
- Infecciones bacterianas – Greenish nails, often seen in salon clients, are usually caused by a Pseudomonas bacterias en lugar de hongos.
- Envejecimiento de las uñas – As we age, our nails naturally thicken and become more brittle, which can sometimes mimic fungal changes.
If you’re unsure whether a client has a fungal infection or another condition, do not attempt to diagnose it yourself. Remember, accurately identifying nail fungus in the salon is crucial for appropriate referral to a podiatrist for proper testing and confirmation.
¿Qué debe hacer si detecta hongos en las uñas en el salón de belleza?
1. No realice ningún tratamiento en la uña afectada
It’s tempting to try and cover up a discoloured nail that may or may not be a fungal infection with polish or gel, but that won’t solve the problem. In fact, it can make things worse by trapping moisture and encouraging fungal growth. Plus, working on an infected nail puts your clients at risk especially if they are not properly cleaned and disinfected.
Instead, gently explain to the client what you’ve noticed and recommend they seek professional advice.
2. Desinféctelo todo
Fungal infections spread through tiny spores, which can linger on tools, nail files, and in footbaths. To prevent cross-contamination:
- Lave primero todas las herramientas y superficies metálicas con agua y jabón
- Utilice desinfectantes de uso hospitalario en todas las superficies y herramientas metálicas.
- Dispose of single-use items like nail files and buffers.
- Limpiar correctamente los lavapiés entre cliente y cliente.
3. Asesorar al cliente sobre los próximos pasos
If you suspect a fungal nail infection, advise your client to visit a podiatrist. Many people don’t realise that fungal infections need medical treatment, simply cutting or filing the nail won’t make it go away. The only way to be sure it is a fungal infection is to test for it.
Opciones de tratamiento para los hongos en las uñas
Una vez diagnosticadas, las clientas tienen diversas opciones de tratamiento. Como técnico de uñas, conocer estos tratamientos te ayudará a educar a tus clientas y apoyarlas en su camino hacia la salud de las uñas.
1. Antifúngicos tópicos (lacas, cremas y soluciones)
Se aplican directamente sobre la uña y pueden ayudar en casos leves, aunque requieren un uso regular durante meses. Las opciones más populares son:
- Amorolfina (Loceryl) – A medicated nail lacquer.
- Terbinafine (Lamisil)- Un potente spray antifúngico
- Ciclopirox (Curanail) – Another antifungal varnish.
- Tea Tree Oil & Natural Remedies – Some clients swear by them, but results vary.
2. Medicamentos antimicóticos orales (sólo con receta)
For more severe cases, podiatrists may prescribe oral antifungals like:
- Terbinafina – One of the most effective options, usually taken for 3–6 months.
- Itraconazole (Sporanox) – Another option, often used for those who can’t take terbinafine.
3. Terapia láser
Some clinics offer laser treatment to target fungal infections. This can be effective, but it’s expensive and not always widely available and again results vary.
4. Extracción de uñas (en casos extremos)
Si la infección es grave, el podólogo puede recomendar la extirpación completa de la uña. Esto permite tratar directamente el lecho ungueal y evita que el hongo se siga extendiendo.
Cuándo acudir al podólogo
As a salon professional, you’re not expected to diagnose or treat fungal infections—but you can play a vital role in guiding your clients to the right help.
Remitir a un cliente a un podólogo si:
- La uña está engrosada, descolorida o se desmorona.
- La infección se está extendiendo a varias uñas.
- El cliente ha tenido la infección durante mucho tiempo sin mejoría.
- The client has diabetes or poor circulation (these conditions increase the risk of complications).
- La uña se levanta o causa dolor.
Los podólogos pueden confirmar si se trata de hongos (mediante pruebas de laboratorio si es necesario) y ofrecer el tratamiento más adecuado.
Reflexiones finales: Cómo proteger a sus clientes y su salón
Fungal nails are a common but often overlooked issue in salons. As a professional, your job isn’t just to make nails look pretty—it’s also to protect your clients’ health.
By learning to recognise possible fungal infections, maintaining strict hygiene standards, and referring clients to podiatrists when needed, you’re setting yourself apart as a knowledgeable and responsible nail technician.
And let’s be honest, nobody wants fungus ruining their flawless pedicure. So, stay vigilant, educate your clients, and keep your salon a fungus-free zone.