What Nail Professionals, Parents & Carers Need to Know
Autumn and spring bring more than just cosy jumpers and daffodils, they also usher in viral bug season, with hand–foot–mouth disease (HFMD) often leading the charge. One after‑effect that raises eyebrows among nail professionals and parents alike is onychomadesis and hand foot mouth disease, where sudden nail shedding follows the infection. In this article, we’ll untangle the science, share care advice and answer the most common questions, so you can navigate this nail journey with confidence.
Hand Foot Mouth Disease at a Glance
Hand foot mouth disease, primarily caused by the Coxsackie A16 virus, affects mostly children but can hit adults too. It typically presents with:
- A fever that sneaks in before any rash
- Red, painful mouth ulcers
- A tell‑tale rash or blisters on the hands, feet, and sometimes around the buttocks
Interestingly, some individuals show no symptoms at all, yet, weeks later, they find their nails behaving oddly. In many cases, HFMD is clinically confirmed via a throat swab or stool sample to pinpoint the virus.
Onychomadesis Explained: How Hand Foot Mouth Disease Affects Nail Health
Simply put, onychomadesis is the complete separation or shedding of the nail plate from the proximal end, closely following a period when the nail matrix stops functioning properly. That can occur due to:
- High fever
- Systemic viral infection (e.g. HFMD)
When the nail matrix goes quiet, the new cells it produces are weakened. Once it reboots, the fresh nail plate slides under the old, brittle section and pushes it away.
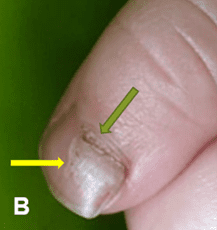
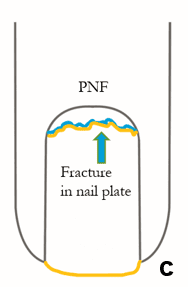
Visuals often help make sense:
- Fig A: Shows a green‑tinged new plate emerging as the yellow, detached old plate loosens
- Fig B: A baby’s tender toes with similar proximal lifting
- Fig C: A side‑view drawing highlighting where separation begins

Though alarming, the good news is that this reaction is temporary. The key is distinguishing it from conditions like fungal infections, which require lab tests to confirm.
Timeline for Nail Changes
Children: Nail changes typically emerge three to four weeks after HFMD
- Adults: The delay can extend to around six weeks
- Affected digits: The issue might involve a single nail or all nails on hands and feet
Why the delay? Nails grow slowly, so the disruption in the matrix takes a few weeks to make itself visible.
Onychomadesis After HFMD: How to Care for Nails During Recovery
Proactive yet gentle care supports smooth recovery:
- Hygiene First
Wash nails and surrounding skin thoroughly with soap and warm water; dry completely. - Shield with Nail Wraps
Self‑adhesive, breathable wraps help:- Gently hold the separated nail plate close to the nail bed
- Prevent it from catching on sheets, clothing, or hair strands, which could cause further lifting or discomfort
- Neaten Sharp Bits
Use a clean sponge file only on sharp splinters, leave solid nail intact. - Trim Carefully
If a hangnail appears, trim it cleanly instead of pulling it; the new nail plate is doing its job underneath. - Avoid E‑Files or Harsh Tools
Baby and child nails are delicate, no electric filing or over‑filing. - When to Escalate
Seek GP or dermatologist input if there’s:- Signs of infection (redness, pain, discharge)
- Pain disproportionate to appearance
- No confidence in managing the nail at home
What Nail Pros Should Share
Educate clients or parents with easy‑to‑understand guidance:
- This nail drop‑off is a natural reaction to systemic stress like HFMD.
- Reassure them: the new nail usually grows back normally.
- Recommend simple hygiene, protection, and patience rather than aggressive interventions.
Real‑World FAQs
1. Why is my child’s nail falling off after a virus?
Onychomadesis is a known nail reaction following high fever or viral infections like HFMD. The nail matrix pauses, then restarts, pushing the weakened portion forward until it sheds.
2. Toenail falling off weeks after hand, foot and mouth – should I worry?
No need to panic! It’s common three to six weeks post‑HFMD. Keep it clean, wrap it if needed, and watch for infection signs.
3. Is it normal for nails to separate after HFMD?
Yes—up to one in ten children with HFMD experience onychomadesis and hand foot mouth disease effects. The new nail usually grows in normally.
4. Nail lifting after fever – fungal infection or virus?
It often mimics fungal infection. Only a lab test (nail clipping or swab) can confirm fungus.
5. How do I treat onychomadesis in toddlers?
Practice gentle hygiene, apply breathable wraps, trim loose edges, not rip them, and steer clear of harsh nail tools. If you see infection signs, consult a GP.
Myths vs Facts: Onychomadesis and Hand Foot Mouth Disease Nail Loss
- Methacrylate wraps help: Yes, they can provide protection, but go for breathable, self‑adhesive types.
- Filing speeds recovery: No, over‑filing damages the matrix and delays regrowth.
- All infected nails need antifungals: Absolutely not, viral nail shedding isn’t fungal. Treat the virus, not with antifungal meds.
When to See Medical Pros
Although onychomadesis and hand foot mouth disease nail loss is typically harmless, red flags include:
- Painful swelling, redness, or pus
- A nail that doesn’t reattach or regrow within six months
- Multiple nails showing worrying signs
- Underlying conditions like diabetes or immune deficiency
In such cases, immediate referral to a GP or dermatologist is wise.
How to Prevent HFMD and Reduce the Risk of Onychomadesis
While you can’t guarantee prevention, these measures help reduce the risk:
- Emphasise hand hygiene in schools and nurseries.
- Sanitize toys, surfaces, and frequently touched items.
- If HFMD strikes, isolate the infected child until sore mouth and rash resolve.
- Monitor nails in the following weeks and support gently if onychomadesis happens.
Final Thoughts – Onychomadesis and hand foot mouth disease
Onychomadesis and HFMD illustrate how systemic stress shows up in surprising places, like nails. As a nail professional, parent or carer, here’s what to remember:
- The condition is temporary and self‑limiting
- Proper hygiene and gentle care pave the way for healthy regrowth
- Nail shedding often looks worse than it is, brace with reassurance
- Stay informed: up to 10% of children with HFMD may shed nails 3–6 weeks later
When you blend awareness, patience, and simple care, you transform what looks alarming into a manageable, educational moment, showing your client or child that nails bounce back, much like life’s surprises, and they will, too.