Does COVID-19 cause nail disorders?
The short answer is yes, it does. But let’s see what the latest scientific findings report about it.
The new viral infection emerged in 2019 and quickly spread all over the globe.
The initial scientific studies of the new viral nature have led to clear conclusions that the virus causes acute respiratory distress syndrome with a severe impact on cardiovascular and pulmonary systems. Further studies have shown that the virus attacks all systems, including the brain, inner organs, immune system, nerves, blood vessels, and the reproductive system in men. Thus, COVID is currently seen as a systemic infection. Later, the consequences of the active infection were determined in the form of the so-called post-COVID syndrome, which can last from several weeks to several months and even longer. The skin and its appendages, including nails, are clearly involved in many cases.
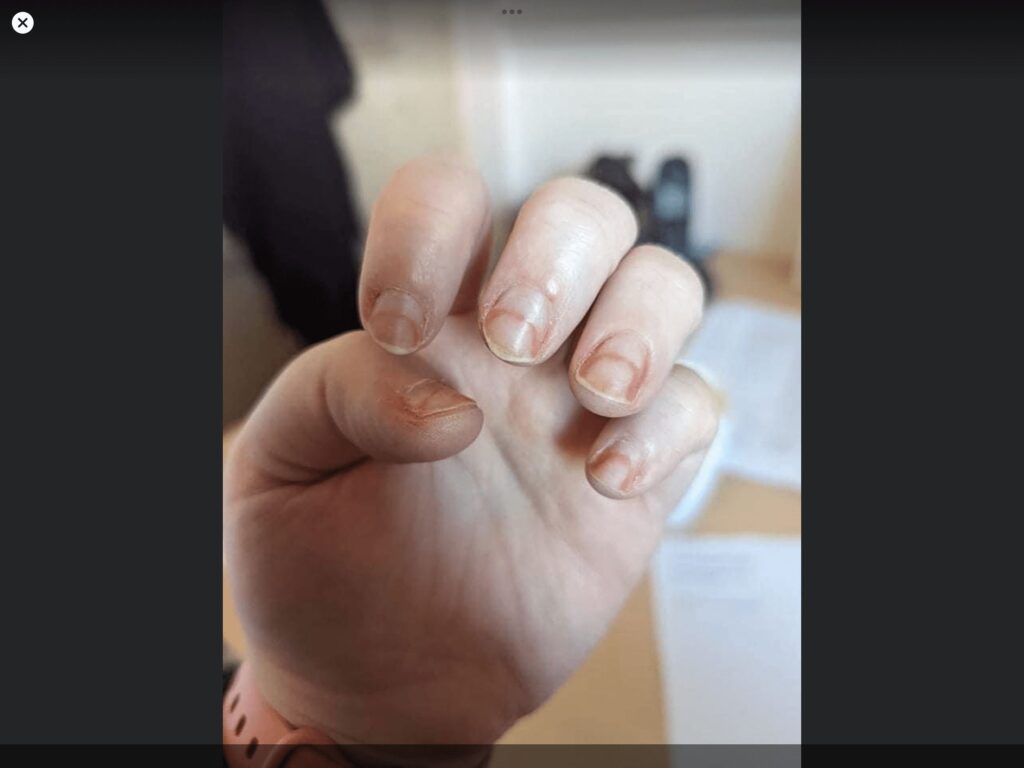
The major outcome caused by COVID is microvascular disturbances when the virus affects the wall of microscopic blood vessels in the skin and in the living parts of the fingernails. In turn, the affected blood vessels don’t perform their physiological function – the quality of blood supply to the organs. The impaired function appears in a form of many well-known symptoms that also can be the symptoms of many other diseases – onycholysis, onychomadesis, leukonychia, etc. So, if your client who has recovered from the recent COVID infection has some unusual or massive symptoms – be prepared, it can be the symptoms of the post-COVID syndrome.
One of the common conditions caused by COVID even has its own name – Covid Toe or Covid Finger. It looks like swollen red nail folds around the nail bed. It is often accompanied by onycholysis or leukonychia. Interestingly, these adverse symptoms are followed by a mild or even asymptomatic course of COVID. Sometimes hematoma-like lesions and hyperkeratosis of the nail bed are also signs of COVID toe or finger. Severe cases look very similar to frostbites of the fingers if the thrombosis and inflammation of the blood vessels are present.
Surprisingly, the latest studies reveal the fact that some vaccines (Pfizer, Moderna) can cause the COVID toe or Finger in some people too several days after vaccination. The good news is that the condition spontaneously disappears after a couple of weeks.
Another condition is Periungual desquamation. The symptom looks very similar to acute onycholysis when nail plates detach from the nail bed. This is also a sign of very severe COVID among adults recovering from the COVID multisystemic inflammatory syndrome.
All sorts of discoloration are also often reported in the studies. They can manifest in the form of red-white discoloration with onycholysis. Sometimes, discolorations of lunula occur during severe COVID. This symptom has been described as a red-violet band surrounding the distal margin of the nail lunula and has its own name. It is known as a “red half-moon sign”. In many cases, the COVID discolorations are observed in adult patients or seniors. So-called “distal orange discolorations” have been described in the studies as a delayed response several weeks after COVID disease. This sign is a flag for a nail tech’s attention since the client with an orange discoloration should be referred to the doctor, because the orange discoloration can be a symptom of post-COVID anemia. However, you can perform the regular manicure or pedicure and apply the nail polish to camouflage the discolorations. Unfortunately, there is no specific treatment for the post covid nail conditions.
Healthcare professionals often reported the type of occupational nail changes, which occur due to the protective measures (gloves) in clinics during the COVID pandemic. The condition is well known to nail techs too – it is a bacterial disease caused by Pseudomonas Aeruginosa and called the “green nail syndrome”. It appears on healthy natural nails. The nail folds can be involved in the pathological process, too, and loss of the nail cuticle is the main sign of this inflammation.
Unfortunately, COVID as any systemic disease attacks many organs in humans. Now we can see that skin and its appendages are not an exclusion. Regretfully, medical science merely didn’t have enough time to elaborate on the specific treatment for all the nail and skin lesions associated with COVID. At least the recent studies show us the path and hope for the specific cure soon.
The literature that has been used for this review:
- Galván Casas C, Català A, Carretero Hernández G, et al. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol.
- Geizhals S, Lipner SR. Retrospective case series on risk factors, diagnosis, and treatment of Pseudomonas aeruginosa nail infections. Am J Clin Dermatol. 2020
- Chernyshov PV, Kolodzinska L. Prospective study on hand dermatitis in nurses and doctors during COVID-19 pandemic and its improvement by use of adopted recommendations of the European academy of dermatology and venereology task force on contact dermatitis. Dermatol Ther. 2020
- Larenas-Linnemann D, Luna-Pech J, Navarrete-Rodríguez EM, et al. Cutaneous manifestations related to COVID-19 immune dysregulation in the pediatric age group. Curr Allergy Asthma Rep. 2021
- Wollina U, Karadag AS, Rowland-Payne C, Chiriac A, Lotti T. Cutaneous signs in COVID-19 patients: a review. Dermatol Ther. 2020
- Wollina U, Chiriac A, Karadag AS. The dermatological spectrum of COVID-19 disease: cutaneous signs for diagnostics and prognosis and an expanded classification. Open Access Maced J Med Sci. 2020
- Ocampo-Garza SS, Ocampo-Candiani J, Camela E, et al. Nail changes as manifestation of systemic disease in COVID-19 infection. J Eur Acad Dermatol Venereol. 2021
- Natalello G, De Luca G, Gigante L, et al. Nailfold capillaroscopy findings in patients with coronavirus disease 2019: broadening the spectrum of COVID-19 microvascular involvement. Microvasc Res. 2021;
- Gomez-Fernández C, Lopez-Sundh AE, González-Vela C, et al. High prevalence of cryofibrinogenemia in patients with chilblains during the COVID-19 outbreak. Int J Dermatol. 2020
- Kanitakis J, Lesort C, Danset M, Jullien D. Chilblain-like acral lesions during the COVID-19 pandemic (“COVID toes”): histologic, immunofluorescence, and immunohistochemical study of 17 cases. J Am Acad Dermatol. 2020
- Discepolo V, Catzola A, Pierri L, et al. Bilateral chilblain-like lesions of the toes characterized by microvascular remodeling in adolescents during the COVID-19 pandemic. JAMA Netw Open. 2021
- Hébert V, Duval-Modeste AB, Joly P, et al. Lack of association between chilblains outbreak and severe acute respiratory syndrome coronavirus 2: histologic and serologic findings from a new immune assay. J Am Acad Dermatol. 2020
- Koschitzky M, Oyola RR, Lee-Wong M, Abittan B, Silverberg N. Pediatric COVID toes and fingers. Clin Dermatol. 2021
- Kashetsky N, Mukovozov IM, Bergman J. Chilblain-like lesions (cll) associated with COVID-19 (“COVID toes”): a systematic review. J Cutan Med Surg. 2021
- Daneshjou R, Rana J, Dickman M, Yost JM, Chiou A, Ko J. Pernio-like eruption associated with COVID-19 in skin of color. JAAD Case Rep. 2020
- de Masson A, Bouaziz JD, Sulimovic L, et al. Chilblains is a common cutaneous finding during the COVID-19 pandemic: a retrospective nationwide study from France. J Am Acad Dermatol. 2020
- König N, Fiehn C, Wolf C, et al. Familial chilblain lupus due to a gainof-function mutation in STING. Ann Rheum Dis. 2017
- Chaudhary H, Mohan M, Jain A, et al. Acral gangrene: ugly cousin of “COVID toes” in multisystem inflammatory syndrome in children associated with SARS-COV-2 Pediatr Infect Dis J. 2021
- Asakura H, Ogawa H. COVID-19-associated coagulopathy and disseminated intravascular coagulation. Int J Hematol. 2021
- Michaud M, Pourrat J. Cryofibrinogenemia. J Clin Rheumatol. 2013
- Feldstein LR, Tenforde MW, Friedman KG, et al. Characteristics and outcomes of US children and adolescents with multisystem inflammatory syndrome in children (MIS-C) compared with severe acute COVID-19. Jama. 2021
- Nakamoto T, Ishikane M, Sasaki R, Ohmagari N. Periungual desquamation in a Japanese adult recovering from severe COVID-19. Int J Infect Dis. 2021
- Abrams JY, Oster ME, Godfred-Cato SE, et al. Factors linked to severe outcomes in multisystem inflammatory syndrome in children (MIS-C) in the USA: a retrospective surveillance study. Lancet Child Adolesc Health. 2021;5(5):323-331.
- Wolf GK, French LE. Beau-lines of the fingernails in association with pediatric SARS-CoV-2 infections. J Dtsch Dermatol Ges. 2021;19(5): 744-745.
- Ide S, Morioka S, Inada M, Ohmagari N. Beau’s lines and leukonychia in a COVID-19 patient. Intern Med. 2020;59(24):3259.
- Alobaida S, Lam JM. Beau lines associated with COVID-19. CMAJ. 2020;192(36):E1040.
- Senturk N, Ozdemir H. Onychomadesis following COVID-19 infection: is there a relationship? Dermatol Ther. 2020;33(6):e14309.
- Hadeler E, Morrison BW, Tosti A. A review of nail findings associated with COVID-19 infection. J Eur Acad Dermatol Venereol. 2021. https://doi.org/10.1111/jdv.17448
- Demir B, Yuksel EI, Cicek D, Turkoglu S. Heterogeneous red-white discoloration of the nail bed and distal onycholysis in a patient with COVID
- Wollina U, Kanitakis J, Baran R. Nails and COVID-19 – A comprehensive review of clinical findings and treatment. Dermatologic Therapy.