How Can We Help?

Onycholysis
159.0k Views
Onicólisis
¿Qué es la onicólisis y cuáles son sus causas?
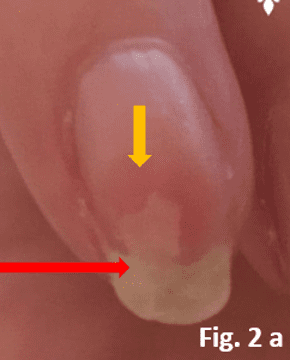
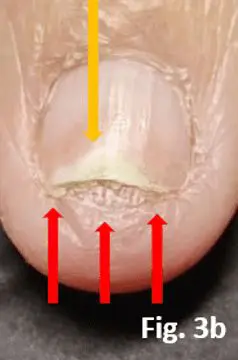
Onycholysis, the separation of the nail plate from the nail bed, can be a painful condition. It is caused by the nail bed responding to an irritation an allergen or mechanical damage by creating keratinous structures and cornifying nail bed epithelium. This separates the nail from the nail bed, forming a cavity where infectious micro-organisms can quickly grow, in some cases may prevent this new formed cornified layer from healing, which may cause the Onycholysis to persist. In the absence of a cornified layer, onycholysis would be expected to disappear as the nail plate grows.
¿Cuáles son las causas de la onicólisis?
Esta afección puede deberse a varias causas:
– mechanical factors. This can happen if the strong seal, the hyponychium, is broken by something being pushed under the free edge. This can be by accident or it could be an aggressive cleaning implement under the free edge. Wearing very long nail enhancements can create a lever effect that can be the cause of onycholysis or may prevent this condition from healing.
– infections. If the hiponiquio seal is broken it is possible that pathogens can enter and infect the nail bed. It is also possible for a pathogens to enter the nail bed from the proximal end of the nail plate under the proximal nail fold. It can be fungal or bacterial. Fungal infections in fingernails are not something we see often, in toenails, fungal infections are more common simply because your shoes are a cosy, warm, dark place that suits a fungal spoor, in most cases, the seals protecting the nail bed are broken. Fungal infections in fingernails are not something we see often, in toenails fungal infections are more common simply because your shoes are a cosy, warm, dark place that suits a fungal spoor, in most cases the seals protecting the nail bed are broken. If the infection is in the nail matrix, it can grow out with the new growth of nail plate and is a condition that can only treated by a healthcare professional.
– irritation/allergies. If anywhere on or in the nail unit there is the presence of a substance that is causing an irratation or allergic reaction, the nail bed epithelium can keratinise to help protect the nail bed and the nail matrix. This can often be one of the early signs that an allergic reaction is present. This used to be a condition only treated by a healthcare professional, but action taken in the salon by a nail technician when this is first spotted can prevent the problem from becoming worse.
The moment the affected nail is recognized all nail coatings need to be removed and the natural nail shortened even if the cause of the onycholysis is not known, long fingernails are prone to accidents especially if they are no longer attached to the nail bed.
– excessive temperatures such as ‘heat spike‘. A ‘heat spike’ (or exothermic reaction’) can be so severe that it burns the nail bed. If this happens the burned area will keratinise and cause the nail plate to separate. Although onycholysis is usually seen under the free edge, it can also be evident in the centre of the nail bed.
– improper structure of artificial enhancements. By this, it means that the structure on the nail is causing too much pressure and lifting the nail plate from the lecho ungueal. A common cause of this is ‘pinching’. This is safe to do on the free edge of the structure if gentle, but when this pressure is exerted over the nail bed with too much force, the nail plate is lifted away from the centre of the nail bed. Another possible cause is a nail tip that has a deeper ‘c’ curve than the natural nail. Even if flattened out during application, the tip will revert to its natural shape and exert upward pressure on the sides of the nail and have a similar effect to pinching.
Afecciones cutáneas existentes o nuevas que causan problemas en las uñas
Another underlying cause of onycholysis could be an existing health condition such as Psoriasis, Alopecia, Lichen Planus or even Eczema. Any one of these common skin conditions can cause a problem for the nail matrix when it is creating our new nail plate cells causing visible problems in the nail plate and/or the nail bed can also be affected.
Psoriasis ungueal normally affects only the upper surface of the nail plate and does not cause pain, but in extreme cases can be painful if small blisters (that look like oil slicks on the surface of the sea) appear underneath the nail plate in the nail bed itself. As this blister swells it triggers the small nerve endings that are abundant in our epidermis layer, this is painful, and relief only comes when the blisters burst and because of these lesions, a secondary infection is always possible. It’s important to maintain nail unit integrity, keep hands and fingers clean and oiled.

Alopecia Areata affects the nail units of up to 46% of sufferers, pitted lines, nail plate splitting, and/or white spots are common and can affect any or all of the nail plates, it is extremely unpleasant and painful. The nail surface is uneven, rough, and full of loose nail plate cells. Filing the upper nail surface will cause the nail plate to unravel causing even more problems, it’s important to maintain nail unit integrity, keep hands and fingers clean and use a good nail and skin oil.

Liquen plano affects the nail plates and the nail bed – The nail bed tissue is not stable and extremely painful to the touch – These clients need approval from a health care specialist or MD and you need to be well versed in artificial nail product application on vulnerable nails, do not help these clients without a full understanding of all the issues, the chances of secondary infection are high and effective treatment takes time and cooperation from the client.

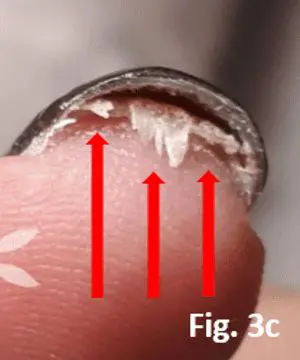
– Hiperqueratosis happens when our skin cells feel the need to defend our epidermal layer usually in our nail bed. Hyperkeratosis is always a reaction to a solvent or uncured product that penetrates the nail plate also excessive use of primers or bonds or a gel product containing uncured monomers that leak out after improper curing or even nail glue can cause this reaction.
¿A quién afecta la onicólisis?
Cualquiera.
¿Cómo pueden ayudar los técnicos de uñas?
Severe cases must be referred to a doctor, especially if signs of bacteria infection, onychomycosis or inflammation are visible.
– mechanical factors: be gentle when cleaning under the free edge and advise clients to do the same.
- infecciones: Avoid damaging the hyponychium seal and keep all tools clean and disinfected/sterilised. If an infection is suspected refer the client to a medical practitioner. A fungal infection can only be determined by medical testing. There are other conditions that can be mistaken for a fungal infection.
- irritaciones o alergias: If there is any sign of an irritation or allergic reaction at all, remove all products and do not reapply until the irritant or allergen has been identified and the nail is healthy.
- pico de calor: This is avoidable if the correct nail lamp that matches the UV gel systems are used and by avoiding applying thick layers of UV gel. If it does occur, the fingers should be removed from the lamp immediately. Sensitive clients can put their nails in the glow of the UV for a few seconds before putting them into the lamp. This will slow down the reaction that is causing the excessive heat.
- la estructura inadecuada de las mejoras artificiales: Evite cualquier procedimiento o estructura que ejerza presión sobre el lecho ungueal.
Las uñas deben mantenerse cortas, limpias y secas, y no debe aplicarse ningún producto para uñas artificiales ni ningún recubrimiento de uñas que necesite curarse.
If a fungal infection is suspected, it can only be confirmed by (a dermatologist after) testing. Una infección por hongos en las uñas no puede verse sólo con el ojo, ya que hay más afecciones de las uñas y de la piel, como la psoriasis ungueal, que tienen el mismo aspecto.
Si se sospecha una alergia, deben retirarse todos los productos de todas las uñas y someter a la clienta a pruebas de alergia para descubrir exactamente qué ingrediente es el causante.
Allergic Contact Dermatitis is a condition that needs to be diagnosed by a health care professional as there could be underlying health conditions or skin conditions that make an allergy more likely – for instance, they could be undergoing chemotherapy or immunotherapy and the medication that they have could affect the skin cell production in such a way that the skin is thinner than normal and more sensitive to medical skin conditions and or skin reactions, that under normal circumstances wouldn’t cause a problem and an allergic reaction is more likely to happen.
Do not suggest tea tree oil! This can be an irritant or allergen and could make the problem worse.
Nail technicians are not health care specialists and should never diagnose a condition but … there are things that we can do in the salon and at home when we see that Onycholysis has occurred.
Debido a que la lámina ungueal se separa del lecho ungueal, es posible que los patógenos se introduzcan por debajo de la lámina ungueal e infecten el lecho ungueal, empeorando el problema. Queremos asegurarnos de que la lámina ungueal separada vuelva a unirse al lecho ungueal sin que se produzcan otras infecciones ungueales (fúngicas o bacterianas) y que la unidad ungueal se recupere.
Protocolo de cuidado de manos y uñas después de la onicolisis en casa:
- Eliminar todos los recubrimientos de uñas
- Lavarse las manos con agua y jabón, secarse bien
- Oil using a good quality nail & skin oil under the free edge – doing this will cause the bed epithelium (non-living tissue that keeps the nail plate attached to the nail bed) to become elastic again and stop the space being a good place for infections to start
Repita estos pasos 4 -5 veces al día
- Vigila la uña, si cambia de color acude a un profesional sanitario, podría ser el inicio de una infección bacteriana (esta es la razón por la que no se debe poner un recubrimiento de color en la uña, cuanto antes se detecte una infección más rápido se podrá tratar).
- Intente vivir sin recubrimientos de uñas hasta que la placa ungueal se vuelva a unir al lecho ungueal.
Protocolo de cuidado de manos/uñas tras onicólisis en el salón de manicura:
- Retire todos los recubrimientos de uñas.
- Take pictures of the affected nail – write the time & date and record the products used.
- Lávese las manos con agua y jabón, y séquelas bien.
- Aceite, Utilice un aceite de buena calidad para uñas y piel debajo del borde libre, esto hará que el epitelio del lecho (tejido no vivo que mantiene la placa ungueal unida al lecho ungueal) se vuelva elástico de nuevo y evitará que el espacio sea un buen lugar para que comiencen las infecciones, dele esto a su cliente para que continúe usándolo en casa.
- No sustituya el recubrimiento de la uña hasta que la placa ungueal se haya vuelto a unir al lecho ungueal.
- Pida al cliente que vuelva para una revisión dentro de una semana.
- Vigila la uña, si cambia de color acude a un profesional sanitario, podría ser el inicio de una infección bacteriana (esta es la razón por la que no se debe poner un recubrimiento de color en la uña, cuanto antes se detecte una infección más rápido se podrá tratar).
- Haz nuevas fotos y entrégaselas a tu cliente para que pueda enseñárselas al profesional sanitario o al médico.
If your client or customer needs to attend a wedding or function, of course, he/she wants amazing looking nails, please use only a quality nail varnish / nail polish for the occasion and remove it after the function or party – taking time now to ensure an infection doesn’t happen or is spotted on time will ensure that he/she can return to their favourite nail coating sooner.
¿Puede la onicólisis ser un signo de trastornos tiroideos?
Descubre cómo trastornos tiroideos can impact nail health, specifically leading to onycholysis. Learn about the signs nail professionals should look for to better understand and manage these conditions.
Galería Onicólisis